Researchers looking into retinitis pigmentosa have been able to improve vision in rats using the CRISPR-Cas9 gene editing technology. Retinitis pigmentosa is an inherited retinal condition that gradually reduces vision over years as the retinal cells die. It starts with loss of night vision and peripheral vision, leading to deterioration of the detailed vision needed for reading, the central vision that allows people to see straight ahead, and the colour vision. It affects around one in 4000 people in the USA and Europe and there is no cure.
The particular form of retinitis pigmentosa the team treated is caused by an error in one of the two copies of a key gene: humans normally have two identical copies of each gene. The gene mutation results in the sight loss, and such a relatively simple genetic error ought to be a natural target for CRISPR-Cas9 therapy given that this approach allows very directed DNA editing. However, CRISPR-Cas9 requires dividing cells to produce the requisite nucleases to edit the DNA and the challenge has been to edit genes in non-dividing cells, which make up most adult tissues.
Recent work has shown a route to use CRISPR-Cas9 in non-dividing cells. The body’s own DNA protection usually uses homology-directed repair, which requires matching of a longer stretch of gene sequences between the damaged DNA and the intact 'donor' DNA. It maintains genomic stability by repairing broken DNA strands and is assumed to be error free because of the use of a template. However, it is only effective when cells are dividing. In this case the Salk Institute and others used homology-independent targeted integration via the non-homologous end joining (NHEJ) mechanism which is also active in non-dividing cells. While this can be a more error-prone approach to CRISPR-Cas9, as it matches a much shorter strand of DNA, it has potential to work in both dividing and non-dividing cells in vitro and in vivo.
“Using this NHEJ pathway to insert entirely new DNA is revolutionary for editing the genome in live adult organisms,” says Keiichiro Suzuki of the Salk Institute. “No one has done this before."
The researchers used adeno-associated virus (AAV) vectors to deliver HITI constructs including a functional copy of the faulty Mertk gene to the eyes of three-week old rats. They were able to restore a degree of vision, allowing the animals to respond to light. The research was published in Nature.
“We are very excited by the technology we discovered because it’s something that could not be done before,” says Juan Carlos Izpisua Belmonte of the Salk Institute's Gene Expression Laboratory. “For the first time, we can enter into cells that do not divide and modify the DNA at will. The possible applications of this discovery are vast.”
One of the key advantages of the HITI approach, as well as its ability to work in non-dividing cells, is that it could be adapted to work with other targeted genome engineering systems, not just CRISPR-Cas9. The next step will be to improve the delivery efficiency of the HITI construct.
As well as providing hope for people with genetically-related sight loss, these approaches could have applications in a wide range of genetic targets in the brain, heart and liver, as well as other genetic disorders such as muscular dystrophy, haemophilia and cystic fibrosis, by either correcting the gene or replacing it with a new one.
While no clinical trials have yet begun in Europe or the US, researchers in China have begun the world's first clinical trial in humans, knocking out the (programmed cell death protein-1) gene in people with non-small cell lung cancer (NSCLC).
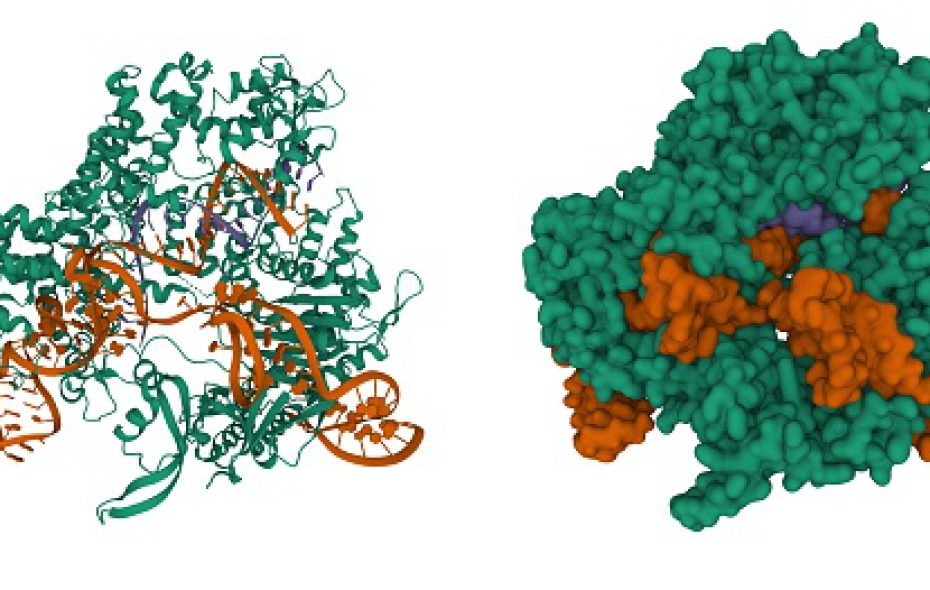
Image supplied by Salk Institute.